 Rome Campus
Rome Campus
18 Courses
Grand Rounds
Highlights of Lead Papers from the Rome Foundation Global Epidemiology Study
A Rome Foundation Continuing Medical Education program
The groundbreaking Rome Foundation Global Epidemiology Study (RFGES) has now published over 40 papers with many others in preparation.
It serves as the reference paper for practice and research on the Disorders of Gut-Brain Interactions (DGBI) and its initial paper “Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study” is now approaching 1,000 citations, making it the leading reference in the field.
In this session of the Rome Foundation Grand Rounds, we will present an introduction to the RFGES and its methodology and highlight three of its leading papers:
-Greater Overlap of Rome IV Disorders of Gut-Brain Interactions Leads to Increased Disease Severity and Poorer Quality of Life. Presenter, Ami Sperber
-Novel Irritable Bowel Syndrome Subgroups are Reproducible in the Global Adult Population. Presenter, Chris Black
-Symptom profiles compatible with disorders of gut-brain interaction (DGBI) in organic gastrointestinal diseases: A global population-based study. Presenter, Tom van Gils
Presented by:
Ami Sperber, MD, MSPH, RFF
Olafur Palsson, PsyD
Chris Black, PhD, MRCP
Tom van Gils, MD PhD

Grand Rounds
Grand Rounds 2024 - Scientific evidence for a central role of food in IBS
This symposium from the newly formed Rome Foundation Diet and Nutrition section provides updates about the scientific evidence that supports the relevance of food in symptom generation in IBS and the use of various dietary interventions in the management of patients with IBS.
The symposium starts with a general overview on the role of food in the pathophysiology with IBS by Rome Foundation Board Member Magnus Simrén, University of Gothenburg, Sweden, and continues with two lectures dedicated to the current dietary interventions used to treat symptoms in IBS by Caroline Tuck, Swinburne University, Australia and Stine Störsrud, University of Gothenburg, Sweden; the session ends with a general discussion and Q&A, and after the session attendees will have a better knowledge about the scientific basis for a central role for food in the pathophysiology in IBS, and for use of dietary approaches as part of the clinical management of IBS, and how to communicate this to the patients.
Presented by:
Magnus Simrén, MD, PhD, RFF
Carolina Tuck, PhD
Stine Störsrud, RD, PhD
Grand Rounds
Grand Rounds 2024 - Low FODMAP Diet Dilemmas: A Case-based Approach
This symposium will use a case-based approach to provide answers to questions that commonly arise about the low FODMAP diet when used for patients with IBS:
|
Presented by:
William D. Chey, MD, AGAF, FACG, FACP, RFF
Marvin Pollard, Professor of Gastroenterology, Professor of Nutrition Sciences
Chief, Division of Gastroenterology & Hepatology
Michigan Medicine, Ann Arbor, MI, USA
Nancee B. Jaffe, MS, RDN
Lead Dietitian for the UCLA Vatche and Tamar Manoukian Division of Digestive Diseases

Grand Rounds
Grand Rounds 2024: The 3 step approach to Integrated Psychosocial Care in DGBI
Objectives for this Grand Rounds include:
|
Presented by:
Laurie Keefer, PhD, RFF
Professor of Medicine and Psychiatry
Icahn School of Medicine at Mount Sinai
New York, NY, USA

Grand Rounds
Grand Rounds 2024: Abdominal Bloating and Distension
This Rome Foundation Grand Rounds presentation will appeal to individuals interested in evaluating and treating one of the most prevalent cluster of gastrointestinal symptoms – gas and bloating. These symptoms develop for a variety of different reasons. They are reported by a large number of patients with disorders of gut-brain interaction, such as irritable bowel syndrome and functional dyspepsia. The cause can be elusive; the pathophysiology is complex. The speaker will provide his perspective on this disorder, based on his clinical experience treating patients with these symptoms and research in the field.
Objectives for this Grand Rounds include:
● Review the epidemiology of abdominal bloating and distension
● Appreciate the complex pathophysiology of bloating and distension
● Recognize available treatment options
Speaker:
Brian E. Lacy, MD, PhD, FACG, RFF
Professor of Medicine & Senior Associate Consultant
Mayo Clinic, Jacksonville, FL, USA

Grand Rounds
Grand Rounds 2024: Ten Questions About Functional Dyspepsia (An Interactive Case-based Illustration of New Developments)
Functional dyspepsia is one of the most common and challenging conditions in clinical practice. The last few years have seen major evolutions in the understanding of the disease, its underlying pathophysiology, and the available treatment options. The separation from gastroparesis is an ongoing topic of transatlantic and international debate.
This interactive program will use a case-based approach to reveal some of the current concepts, ongoing controversies, and new information that is likely to be presented at meetings and in the literature later this year.
The program will appeal to clinicians, medical providers, and researchers interested in understanding the complexity of upper gastrointestinal symptoms, their relationship to physiological events such as food intake, and the potential impact of novel pharmacological and dietary therapeutic interventions.
Grand Rounds
Grand Rounds 2024: Abuse, Trauma, and Illness: What is the link?
A Rome Foundation Continuing Medical Education program
Presentation by Douglas A. Drossman, MD With special guests: Lin Chang MD & Johannah Ruddy MEd
This comprehensive program will appeal to individuals interested in unraveling the intricate interplay between abuse, trauma, and gastrointestinal illness.
Part 1 begins with a compelling case report by Dr. Drossman, recounting the journey of his adolescent patient who, having endured early trauma, developed gastrointestinal symptoms. This case spurred Dr. Drossman to pioneer the first study in the medical literature, elucidating this association.
Part 2, presented by Dr. Chang, offers an insightful research update, including her groundbreaking studies into the association between adverse childhood events and gastrointestinal illness, bringing us to the present day.
Part 3, presented by Ms. Ruddy, invites us into the realm of a patient’s experience.
Part 4 concludes the program as Dr. Drossman imparts his clinical experience and insights in caring for these patients to aid healthcare providers.

Grand Rounds
Grand Rounds: Communication Skills
Have you felt challenged when communicating with your patient or even frustrated that the visit just isn’t going well? Now you can learn Grand Rounds how to successfully navigate complex patient interactions, improving patient provider satisfaction and clinical outcome.
Douglas A. Drossman, MD, a recognized authority in DGBI and communication strategies, will present tips and techniques for optimizing the patient-provider relationship through the medical interview.
Objectives:
●Learners will understand how to provide patient centered care and improve upon shared decision making.
● Learners will understand the importance of effective communication skills to navigate challenging clinical situations
● Learners will understand the impact of DGBI from the patient’s perspective and learn their role in reducing the stigma experience for patients with DGBI

Grand Rounds
Grand Rounds: Sociocultural aspects of the assessment and treatment of patients with DGBI
A Rome Foundation Continuing Medical Education program Awareness and understanding of the sociocultural background of patients with DGBI can help avoid pitfalls and enhance the clinical outcome of patients with DGBI. The Multidimensional Clinical Profile (MDCP) approach, with unique case presentations, will be used to demonstrate how to navigate these complex issues in clinical practice.
Objectives:
● Recognize and assess the patient’s sociocultural background and its potential effect on the patient/HCP relationship and clinical outcome.
● Assess the effect of sociocultural factors on the patient’s “explanatorymodel of illness.”
● Recognize and bridge differences between the patient’s and the provider’s sociocultural backgrounds.
● Use the Multidimensional Clinical Profile (MDCP) approach to clinical practice including sociocultural influences.

Grand Rounds
Grand Rounds: Diet and DGBI
Introducing Rome Grand Rounds Session #4: Diet & DGBI
A virtual, interactive and intensive educational opportunity on topics related to Disorders of Gut-Brain Interaction (DGBI)
Each session will offer 1.25 CME credits and the opportunity to learn from the world’s best clinicians and researchers in the area of DGBI.
Objectives:
● Understand the role that food can play in symptom generation in patients with DGBI.
● Understand the impact that dietary therapies can play in symptom management
● Understand how the integrated care model, include dietary guidance, can improve clinical outcomes

Grand Rounds
Grand Rounds: Post Covid-19 DGBI
Introducing Rome Grand Rounds Session #7: Post Covid-19 DGBI
A virtual, interactive and intensive educational
opportunity on topics related to
Disorders of Gut-Brain Interaction (DGBI)
Each session will offer 1.25 CME credits and the
opportunity to learn from the world’s best clinicians and
researchers in the area of DGBI.
Objectives:
● To understand the mechanisms that explains the impact of SARS-CoV-2 in the GI tract.
● To understand the underlying pathophysiological mechanisms of the Post COVID-19 DGBI and learn the Diagnostic Criteria.”
● To learn the current studies that demonstrate the presence of Post COVID-19 DGBI.
● To review how the COVID-19 pandemic impacted in the practice of Neurogastroenterology especially in terms of Motility and DGBI.

Grand Rounds
Grand Rounds: Evidence supporting Brain-Gut Behavioral Therapies (BGBT) and Integrated Care to Improve access through Mental Health
Objectives:
● Be able to explain the evidence supporting integrated behavioral care in DGBI.
● Identify a model of integrated behavioral care that would a) work in your practice tomorrow and b) could be implemented in your practice over the next two years
● Be able to explain the strengths and limitations of digital technology as part of integrated behavioral DGBI care
Grand Rounds
Grand Rounds: Deep Dive Into Central Neuromodulators
Objectives:
● Explained the pathophysiological basis for central neuromodulators in treating pain and other symptoms in patients with DGBI
● Determined treatment options for patients with DGBI symptoms, including abdominal pain

Grand Rounds
Grand Rounds: DGBI in Pediatric Populations
Objectives:
● Understand the pathophysiology of Pain Predominant Pediatric Disorders of Gut Brain Interaction (DGBI)
● Identify the utility for different treatments including non-pharmacologic and pharmacologic interventions
● Understand the multidisciplinary approach to the treatment of these patients

Grand Rounds
Grand Rounds: Gastroparesis vs FD
Objectives:
● To understand the pathophysiology of both Functional Dyspepsia with sub-categories and Gastroparesis
● To understand the overlapping mechanisms of both conditions, with and without nausea/vomiting
● To understand the recommendations for when/when not to use gastric emptying testing for diagnosis
● To understand the recommendations for treatment of both conditions
Grand Rounds
Grand Rounds: History of Disorders of Gut-Brain Interaction - DGBI (Functional GI Disorders)
This Grand Rounds features the original members of the Rome Foundation board who address the History of DGBI from the last millennia, to the present time. They also discuss the basis for the creation of the Rome Foundation.
Objectives:
● To understand the historical evolution of thinking about DGBI
● To understand the pathophysiological bases for DGBI
● Describe the historical evolution of thinking about DGBI
● Describe the pathophysiological bases for DGBI
● Trace the history of the formation of the Rome Foundation
Grand Rounds
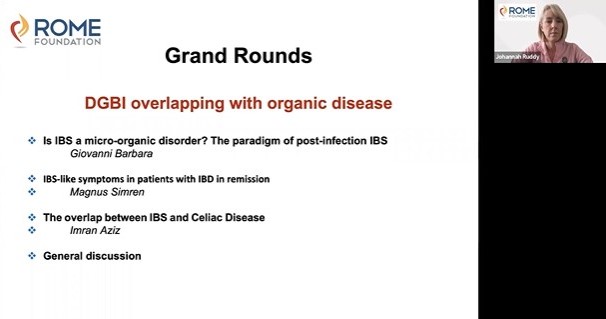
Grand Rounds: DGBI Overlapping with Organic Disease
Objectives:
● Describe the prevalence, GI symptom patterns and clinical impact of coexisting GI illnesses, assess potential geographic and demographic differences, and address how the presence of these symptoms relates to GI symptom patterns in specific DGBI.
● Provide guidance on how the presence of co-existing GI illnesses influences burden of the disease, clinical outcomes and patient management, including how to prioritize different treatment strategies.

Grand Rounds
Grand Rounds: Initial Approach to a Patient with Severe Chronic Abdominal Pain: How to Engage, Educate and Achieve Collaborative Care
This module shows the interaction with Ms. Byers a simulated patient with multiple diagnoses including:
● Post-infection IBS
● Opioid-induced constipation
● Narcotic Bowel Syndrome
● Centrally mediated abdominal pain
● Psychosocial difficulties including
- History of abuse and trauma
- Somatic symptom disorder
- Visceral anxiety
- Depression
- Opioid seeking behavior
This module is designed to help the provider understand these disorders, engage with the patient in an effective patient-provider relationship, and use good communication skills to recommend effective treatments.