 Rome Campus
Rome Campus
GastroPsych Pediatric Clinical Case Conference Series
Rome Foundation GastroPsych Clinical Case Conference Series - Session One
Rome Foundation GastroPsych Clinical Case Conference Series - Session Two
Rome Foundation GastroPsych Clinical Case Conference Series - Session Three
Rome Foundation GastroPsych Clinical Case Conference Series - Session Four
Rome Foundation GastroPsych Clinical Case Conference Series - Session Five
Rome Foundation GastroPsych Clinical Case Conference Series - Session Six
Rome Foundation GastroPsych Clinical Case Conference Series - Session Seven
Rome Foundation GastroPsych Clinical Case Conference Series - Session Eight
Back to School with Disorders of Gut Brain Interactions
Psychosocial and Cultural Considerations in GI Behavioral Health
Psychogastroenterology Basic Skills Workshop - 8 CE credits
Hypnosis Techniques in Psychogastroenterology - 3 CE Credits
Behavioral Interventions for DGBI Conditions of the Upper GI Tract
Cognitive-Behavioral Therapy for Avoidant/Restrictive Food Intake Disorder (ARFID)
GI Physiology for the Behavioral Health Provider - 1.5 CE Credits
2023 Pediatric Symposium: Hot Topics in Pediatric DGBI
Grand Rounds - Demystifying Gastroparesis: Lessons from Around the World
Highlights of Lead Papers from the Rome Foundation Global Epidemiology Study
Grand Rounds 2024 - Scientific evidence for a central role of food in IBS
Grand Rounds 2024 - Low FODMAP Diet Dilemmas: A Case-based Approach
Grand Rounds 2024: The 3 step approach to Integrated Psychosocial Care in DGBI
Grand Rounds 2024: Abdominal Bloating and Distension
Grand Rounds 2024: Abuse, Trauma, and Illness: What is the link?
Grand Rounds: Communication Skills
Grand Rounds: Sociocultural aspects of the assessment and treatment of patients with DGBI
Grand Rounds: Post Covid-19 DGBI
Grand Rounds: Deep Dive Into Central Neuromodulators
Grand Rounds: DGBI in Pediatric Populations
Grand Rounds: Gastroparesis vs FD
Grand Rounds: History of Disorders of Gut-Brain Interaction - DGBI (Functional GI Disorders)
Grand Rounds: DGBI Overlapping with Organic Disease
Grand Rounds - Demystifying Gastroparesis: Lessons from Around the World copy 1
Highlights of Lead Papers from the Rome Foundation Global Epidemiology Study copy 1
Grand Rounds 2024 - Scientific evidence for a central role of food in IBS copy 1
GastroPsych Clinical Case Conference Series
GastroPsych - Integrating Group Therapy into GI Behavioral Health Practice
Grand Rounds 2024 - Low FODMAP Diet Dilemmas: A Case-based Approach
Grand Rounds: The 3 step approach to Integrated Psychosocial Care in DGB
Grand Rounds: Abdominal Bloating and Distension
Grand Rounds: Abuse, Trauma, and Illness: What is the link?
Grand Rounds: ACG vs AGA IBS Guidelines and Clinical Application
GastroPsych Pediatric Clinical Case Conference Series
Rome Foundation GastroPsych Clinical Case Conference Series - Session One
Rome Foundation GastroPsych Clinical Case Conference Series - Session Two
Rome Foundation GastroPsych Clinical Case Conference Series - Session Three
Rome Foundation GastroPsych Clinical Case Conference Series - Session Four
Rome Foundation GastroPsych Clinical Case Conference Series - Session Five
Rome Foundation GastroPsych Clinical Case Conference Series - Session Six
Rome Foundation GastroPsych Clinical Case Conference Series - Session Seven
Rome Foundation GastroPsych Clinical Case Conference Series - Session Eight
Back to School with Disorders of Gut Brain Interactions
Psychosocial and Cultural Considerations in GI Behavioral Health
Psychogastroenterology Basic Skills Workshop - 8 CE credits
Hypnosis Techniques in Psychogastroenterology - 3 CE Credits
Behavioral Interventions for DGBI Conditions of the Upper GI Tract
Cognitive-Behavioral Therapy for Avoidant/Restrictive Food Intake Disorder (ARFID)
GI Physiology for the Behavioral Health Provider - 1.5 CE Credits
Grand Rounds - Demystifying Gastroparesis: Lessons from Around the World
Highlights of Lead Papers from the Rome Foundation Global Epidemiology Study
Grand Rounds 2024 - Scientific evidence for a central role of food in IBS
Grand Rounds 2024 - Low FODMAP Diet Dilemmas: A Case-based Approach
Grand Rounds 2024: The 3 step approach to Integrated Psychosocial Care in DGBI
Grand Rounds 2024: Abdominal Bloating and Distension
Grand Rounds 2024: Abuse, Trauma, and Illness: What is the link?
Grand Rounds: Communication Skills
Grand Rounds: Sociocultural aspects of the assessment and treatment of patients with DGBI
Grand Rounds: Post Covid-19 DGBI
Grand Rounds: Deep Dive Into Central Neuromodulators
Grand Rounds: DGBI in Pediatric Populations
Grand Rounds: Gastroparesis vs FD
Grand Rounds: History of Disorders of Gut-Brain Interaction - DGBI (Functional GI Disorders)
Grand Rounds - Demystifying Gastroparesis: Lessons from Around the World copy 1
Highlights of Lead Papers from the Rome Foundation Global Epidemiology Study copy 1
Grand Rounds 2024 - Scientific evidence for a central role of food in IBS copy 1
GastroPsych Clinical Case Conference Series
GastroPsych - Integrating Group Therapy into GI Behavioral Health Practice
Grand Rounds 2024 - Low FODMAP Diet Dilemmas: A Case-based Approach
Grand Rounds: The 3 step approach to Integrated Psychosocial Care in DGB
Grand Rounds: Abdominal Bloating and Distension
Grand Rounds: Abuse, Trauma, and Illness: What is the link?
Grand Rounds: ACG vs AGA IBS Guidelines and Clinical Application
ALL CME PROGRAMS
GastroPsych Pediatric Clinical Case Conference Series
A Rome Foundation Continuing Medical Education program
CE Credits: 1 hour of continuing education credit for Licensed Psychologists will be awarded for each seminar. Cost for the entire series (6) of programming: $100.00. Attendees must complete each seminar's associated evaluation form in order to receive credit.
This clinical case series will highlight pediatric gastrointestinal (GI) conditions and associated challenges that are commonly encountered by mental health providers in clinical practice. Each seminar will be one hour in length and feature a psychogastroenterology provider presenting on his/her area of expertise. The seminar will include a didactic presentation, including an overview of the medical condition, the rationale for psychological treatment, and the scientific basis for the approach. This will be followed by a case example to illustrate the condition and approach being presented. The program will draw upon current research findings related to the content as well as the clinical practice knowledge of the presenter. The program will conclude with a moderated question and answer session.

Rome Foundation GastroPsych Clinical Case Conference Series - Session One
Psychological Care for Adults with Chronic Pancreatitis
A Rome Foundation Continuing Medical Education program
CE Credits: 1 hour of continuing education credit for Licensed Psychologists will be awarded. There is no cost to attend. Attendees must complete the seminar's associated evaluation form in order to receive credit.
Level: Intermediate
Description:
Patients with a wide range of gastrointestinal conditions, including functional bowel disorders, gastroparesis, chronic pancreatitis, esophageal conditions, and inflammatory bowel disease may experience brain-gut dysregulation that can impact their symptoms and/or disease experience. In an engaging and practical case series, leading experts in psychogastroenterology will discuss how to utilize psychological interventions with complex and unique GI presentations. Each seminar will include a didactic presentation, including an overview of the condition being treated, the rationale for psychological treatment and the scientific basis for the approach. This will be followed by a case example to illustrate the condition and approach being presented. The program will draw upon current research findings related to the content as well as the clinical practice knowledge of the presenter.
Learning Objectives:
1. Describe at least 3 psychosocial factors that influence the experience of pain and quality of life in chronic pancreatitis
2. Explain how to apply cognitive behavioral interventions for patients with chronic pancreatitis

Rome Foundation GastroPsych Clinical Case Conference Series - Session Two
Behavioral Treatment for Sleep Disturbance in DGBIs
A Rome Foundation Continuing Medical Education program
CE Credits: 1 hour of continuing education credit for Licensed Psychologists will be awarded. There is no cost to attend. Attendees must complete the seminar's associated evaluation form in order to receive credit.
Level: Intermediate
Description:
Patients with a wide range of gastrointestinal conditions, including functional bowel disorders, gastroparesis, chronic pancreatitis, esophageal conditions, and inflammatory bowel disease may experience brain-gut dysregulation that can impact their symptoms and/or disease experience. In an engaging and practical case series, leading experts in psychogastroenterology will discuss how to utilize psychological interventions with complex and unique GI presentations. Each seminar will include a didactic presentation, including an overview of the condition being treated, the rationale for psychological treatment and the scientific basis for the approach. This will be followed by a case example to illustrate the condition and approach being presented. The program will draw upon current research findings related to the content as well as the clinical practice knowledge of the presenter.
Learning Objectives:
1. Identify the relationship between poor sleep and disorders of gut brain interaction
2. Describe the key techniques of behavioral treatment for insomnia in DGBIs

Rome Foundation GastroPsych Clinical Case Conference Series - Session Three
Psychological Intervention with Adolescent/Young Adult Patients with DGBIs
A Rome Foundation Continuing Medical Education program
CE Credits: 1 hour of continuing education credit for Licensed Psychologists will be awarded. There is no cost to attend. Attendees must complete the seminar's associated evaluation form in order to receive credit.
Level: Intermediate
Description:
Patients with a wide range of gastrointestinal conditions, including functional bowel disorders, gastroparesis, chronic pancreatitis, esophageal conditions, and inflammatory bowel disease may experience brain-gut dysregulation that can impact their symptoms and/or disease experience. In an engaging and practical case series, leading experts in psychogastroenterology will discuss how to utilize psychological interventions with complex and unique GI presentations. Each seminar will include a didactic presentation, including an overview of the condition being treated, the rationale for psychological treatment and the scientific basis for the approach. This will be followed by a case example to illustrate the condition and approach being presented. The program will draw upon current research findings related to the content as well as the clinical practice knowledge of the presenter.
Learning Objectives:
1. Participants will be able to explain the scientific basis for integrating behavioral health interventions for AYA patients with DGBI diagnoses
2. Participants will be able to discuss characteristics unique to the AYA population that are critical for informing psychological treatment

Rome Foundation GastroPsych Clinical Case Conference Series - Session Four
Behavioral Medicine Interventions for Eosinophilic Esophagitis
A Rome Foundation Continuing Medical Education program
CE Credits: 1 hour of continuing education credit for Licensed Psychologists will be awarded. There is no cost to attend. Attendees must complete the seminar's associated evaluation form in order to receive credit.
Level: Intermediate
Description:
Patients with a wide range of gastrointestinal conditions, including functional bowel disorders, gastroparesis, chronic pancreatitis, esophageal conditions, and inflammatory bowel disease may experience brain-gut dysregulation that can impact their symptoms and/or disease experience. In an engaging and practical case series, leading experts in psychogastroenterology will discuss how to utilize psychological interventions with complex and unique GI presentations. Each seminar will include a didactic presentation, including an overview of the condition being treated, the rationale for psychological treatment and the scientific basis for the approach. This will be followed by a case example to illustrate the condition and approach being presented. The program will draw upon current research findings related to the content as well as the clinical practice knowledge of the presenter.
Learning Objectives:
1. Participants will become knowledgeable about the main psychological effects of eosinophilic esophagitis and its treatments, including illness specific anxiety, food related quality of life, and depression
2. Participants will understand the role of behavioral medicine interventions in the multidisciplinary management of eosinophilic esophagitis including commonly used treatments targeting anxiety, hypervigilance, and esophageal hypersensitivity

Rome Foundation GastroPsych Clinical Case Conference Series - Session Five
Psychological Treatment Strategies for Cyclic Vomiting Syndrome
A Rome Foundation Continuing Medical Education program
CE Credits: 1 hour of continuing education credit for Licensed Psychologists will be awarded for this seminar. There is no cost to attend. Attendees must complete the seminar's associated evaluation form in order to receive credit.
Level: Intermediate
Description:
Patients with a wide range of gastrointestinal conditions, including functional bowel disorders, gastroparesis, chronic pancreatitis, esophageal conditions, and inflammatory bowel disease may experience brain-gut dysregulation that can impact their symptoms and/or disease experience. In an engaging and practical case series, leading experts in psychogastroenterology will discuss how to utilize psychological interventions with complex and unique GI presentations. Each seminar will include a didactic presentation, including an overview of the condition being treated, the rationale for psychological treatment and the scientific basis for the approach. This will be followed by a case example to illustrate the condition and approach being presented. The program will draw upon current research findings related to the content as well as the clinical practice knowledge of the presenter.
Learning Objectives:
1. Describe the etiology and symptoms of cyclic vomiting syndrome
2. Identifying and applying psychological strategies to promote the management and adaptation to cyclic vomiting syndrome

Rome Foundation GastroPsych Clinical Case Conference Series - Session Six
Case Conceptualization and Cognitive-Behavioral Treatment for Avoidant Restrictive Food
A Rome Foundation Continuing Medical Education program
CE Credits: 1 hour of continuing education credit for Licensed Psychologists will be awarded for this seminar. There is no cost to attend. Attendees must complete the seminar's associated evaluation form in order to receive credit.
Level: Intermediate
Description:
Patients with a wide range of gastrointestinal conditions, including functional bowel disorders, gastroparesis, chronic pancreatitis, esophageal conditions, and inflammatory bowel disease may experience brain-gut dysregulation that can impact their symptoms and/or disease experience. In an engaging and practical case series, leading experts in psychogastroenterology will discuss how to utilize psychological interventions with complex and unique GI presentations. Each seminar will include a didactic presentation, including an overview of the condition being treated, the rationale for psychological treatment and the scientific basis for the approach. This will be followed by a case example to illustrate the condition and approach being presented. The program will draw upon current research findings related to the content as well as the clinical practice knowledge of the presenter.
Learning Objectives:
1. Develop a case conceptualization of dimensional avoidant/restrictive food intake symptoms and their interaction with disorders of gut-brain interaction from a cognitive-behavioral framework
2. Understand the basic tenets of exposure-based cognitive-behavioral treatment for avoidant/restrictive intake symptoms

Rome Foundation GastroPsych Clinical Case Conference Series - Session Seven
Acceptance and Commitment Therapy with a patient with Inflammatory Bowel Disease and an Ostomy
A Rome Foundation Continuing Medical Education program
Level: Intermediate
Patients with a wide range of gastrointestinal conditions, including functional bowel disorders, gastroparesis, chronic pancreatitis, esophageal conditions, and inflammatory bowel disease may experience brain-gut dysregulation that can impact their symptoms and/or disease experience. In an engaging and practical case series, leading experts in psychogastroenterology will discuss how to utilize psychological interventions with complex and unique GI presentations. Each seminar will include a didactic presentation, including an overview of the condition being treated, the rationale for psychological treatment and the scientific basis for the approach. This will be followed by a case example to illustrate the condition and approach being presented. The program will draw upon current research findings related to the content as well as the clinical practice knowledge of the presenter.
Learning Objectives:
1. Identify common concerns of patients with inflammatory bowel disease (IBD) referred for psychological and behavioral treatments
2. Describe the structure and core components of Acceptance and Commitment Therapy (ACT) for GI conditions
CE Credits: 1 hour of continuing education credit for Licensed Psychologists will be awarded for this seminar. There is no cost to attend. Attendees must complete the seminar's associated evaluation form in order to receive credit.

Rome Foundation GastroPsych Clinical Case Conference Series - Session Eight
Session Eight: GI illness and Sexual Dysfunction
A Rome Foundation Continuing Medical Education program
Level: Intermediate
Description:
Patients with a wide range of gastrointestinal conditions, including functional bowel disorders, gastroparesis, chronic pancreatitis, esophageal conditions, and inflammatory bowel disease may experience brain-gut dysregulation that can impact their symptoms and/or disease experience. In an engaging and practical case series, leading experts in psychogastroenterology will discuss how to utilize psychological interventions with complex and unique GI presentations. Each seminar will include a didactic presentation, including an overview of the condition being treated, the rationale for psychological treatment and the scientific basis for the approach. This will be followed by a case example to illustrate the condition and approach being presented. The program will draw upon current research findings related to the content as well as the clinical practice knowledge of the presenter.
Learning Objectives:
1. Participants will identify two strategies for assessing sexual issues in GI patient populations
2. Participants will describe a biopsychosocial conceptualization of sexual dysfunction in GI disorders

Back to School with Disorders of Gut Brain Interactions
A Rome Foundation Continuing Medical Education program
Series of 4 virtual, 1-hr On-Demand Webinars
CE Learning Opportunity
Earn up to 4 CE credits
Pediatric disorders of gut-brain interaction (DGBIs; formally called functional gastrointestinal disorders) are common in young people and are often disruptive of daily routines, including school participation. These conditions are most appropriately treated from a biopsychosocial framework. Through this lens, school participation is both a potential source of psychological and social stress that may exacerbate or maintain DGBIs and also a valued functional outcome. As students prepare to return to school, this educational program will prepare healthcare providers to support adaptive school adjustment as part of DGBI management.
For healthcare providers working with youth with DGBIs including functional abdominal pain disorders (e.g., irritable bowel syndrome, functional dyspepsia). This may include physicians, advanced practice nurses, PAs, nursing staff, behavioral health professionals (psychologists, social workers, counselors) and other allied healthcare providers.

Psychosocial and Cultural Considerations in GI Behavioral Health
A Rome Foundation Continuing Medical Education program
In this workshop, we modify and/or expand upon the fundamentals of GI behavioral health to incorporate socioeconomic and cultural considerations, both challenges patients and providers may face, and ways to address them.
This workshop should be of particular benefit to providers delivering care in lower income and/or culturally diverse settings. After reviewing the fundamentals of GI behavioral health, we explain the rationale for this workshop, including the relationship between socioeconomic and cultural factors and mental and physical health care status.
We then discuss the specific challenges that might arise when working with people with gastrointestinal disorders, possible assessment strategies providers may use to explore existence of these challenges, and ways to further expand and/or modify the principles of GI behavioral health to address them. Finally, we illustrate these principles through case examples.

Psychogastroenterology Basic Skills Workshop - 8 CE credits
Learn about the emerging field of psychogastroenterology and how brain-gut psychotherapies, such as cognitive-behavioral therapy and gut-directed hypnotherapy, can improve outcomes and quality of life for many patients with chronic GI disorders.
The Psychogastroenterology Basic Skills workshop will provide mental health practitioners with a foundation for working with patients with Disorders of Gut-Brain Interaction (DGBI), such as irritable bowel syndrome, functional dyspepsia, and functional heartburn. Psychological processes play a key role in the development and maintenance of DGBI and brain-gut psychotherapies are among the most effective treatments for patients. In this introductory workshop, international experts in psychogastroenterology will explain the biopsychosocial model for DGBI and discuss the structure and efficacy behind brain-gut psychotherapies for both adult and pediatric populations. Training will also include guidance on developing a successful integrated GI psychology practice.

Hypnosis Techniques in Psychogastroenterology - 3 CE Credits
Learn about the emerging field of psychogastroenterology and how brain-gut psychotherapies, such as gut-directed hypnotherapy can improve outcomes and quality of life for many patients with chronic GI disorders.
An introduction to Acceptance and Commitment Therapy for Disorders of Gut-Brain Interaction (DGBI) - 7 CE Credits
Acceptance and Commitment Therapy (ACT) is an emerging transdiagnostic psychotherapeutic approach for the treatment of long-term chronic conditions, including Disorders of Gut-Brain Interaction (DGBI), such as Irritable Bowel Syndrome or Inflammatory Bowel Diseases. Using an experiential approach, this session intends to introduce practitioners to the ACT model of case conceptualization in DGBIs. Further to that, a brief description of the model of intervention will also be provided, alongside some brief ACT consistent practices that can be easily incorporated into current patient management.

Behavioral Interventions for DGBI Conditions of the Upper GI Tract
A Rome Foundation Continuing Medical Education program
Psychological and behavioral factors play a key role in developing and maintaining DGBI conditions, including disorders of the upper GI tract. Several complex upper GI disorders can be effectively treated with behavioral interventions delivered by multidisciplinary care team members, including psychologists and speech-language pathologists. In a practical and engaging lecture series, leading experts in psychogastroenterology will discuss the anatomy and physiology of the upper GI tract and behavioral techniques to treat belching disorders, rumination syndrome, and gastroesophageal reflux. Each seminar will include a didactic presentation, an overview of the condition being treated, the rationale for behavioral intervention, and the scientific basis for the approach. The program will draw upon current research findings as well as the presenters’ clinical expertise.
Cognitive-Behavioral Therapy for Avoidant/Restrictive Food Intake Disorder (ARFID)
Individuals with chronic gastrointestinal (GI) conditions are at higher risk for developing Avoidant/Restrictive Food Intake Disorder (ARFID)– particularly individuals with DGBIs and dietary-treated conditions. Co-occurring ARFID can have significant health and psychosocial consequences and impact GI condition management. This in-depth workshop will provide Gastropsych clinicians with up-to-date education on ARFID prevalence in GI conditions, diagnostic criteria, and evidence-based treatment strategies, with a particular focus on the use of cognitive-behavioral therapy for ARFID. This program will benefit the multidisciplinary team of GI clinicians that care for individuals with chronic GI conditions (e.g., dietitians, advance practice providers, gastroenterologists) in addition to GI mental health clinicians.
- List diagnostic criteria for ARFID
- Describe the prevalence of ARFID in common GI conditions
- Describe the fundamentals of CBT-AR
- Describe the application of CBT-AR to ARFID presentations among those with GI conditions
- Summarize data supporting the efficacy of CBT-AR data
GI Physiology for the Behavioral Health Provider - 1.5 CE Credits
By the end of this session, participants will be able to:
● Describe and be able to explain to patients the path of digestion from the mouth to the anus, including the role of the esophagus, stomach, intestines, as well as the role of the liver, pancreas and gall bladder.
● Identify a minimum of 3 common digestive disorders and their etiology.
● Effectively explain the dynamics of defecation to patients, and the potential impact of trauma.
● List lifestyle factors and behaviors that can contribute to digestive disruption.

2023 Pediatric Symposium: Hot Topics in Pediatric DGBI
Learning Objectives:
● Using a case-based approach, to review evidence-based recommendations for the evaluation and management of children with DGBI
● To learn more about new and emerging DGBI diagnoses
● To feel more confident in handling controversial medical issues
• Test or not Test: Endoscopy, Imaging, Breath Testing, Impedance, Motility Testing
• Dietary Management: Chasing the Z score, Enteral Tubes, Specialized Diets
• Therapies: Behavioral / neuromodulators / neurostimulation / alternative
• Too Many Cooks in the Kitchen: The Role of the Gastroenterologist in Overlapping Pain Conditions and other diseases (MALS, MCAS, SFN,EDS, POTS, etc)
● From a multidisciplinary panel, to learn biopsychosocial management methods
Grand Rounds - Demystifying Gastroparesis: Lessons from Around the World
A Rome Foundation Continuing Medical Education program
Summary:
This discussion-style and interactive program will be geared towards practitioners and other individuals interested in learning about advancements in gastroparesis.
Objectives:
1. To understand the clinical spectrum of gastroparesis and differentiation from functional dyspepsia
2. To discuss the role of novel diagnostics such as gastric mapping, FLIP, and full-thickness biopsies
3. To appraise clinical trials and the future of drug development for gastroparesis
These presentations will be followed by a Q&A session and panel discussion.
Part 1: This will be a brief overview of gastroparesis epidemiology and clinical presentation by Dr. Grover. Working with the Gastroparesis Clinical Research Consortium, Dr. Grover has participated in over 60 clinical and translational studies in gastroparesis and is a leading authority on disease mechanisms. He has a busy practice of gastroparesis patients. He will share recent epidemiological studies as well as insights on clinical presentation.
Part 2: Dr. Carbone is an internationally recognized researcher in GI motility disorders and played key roles in developing international consensus statements on gastroparesis and functional dyspepsia. Using a case-based approach, Dr. Carbone will lead discussion on the diagnosis of gastroparesis, challenges with gastric emptying study and how to conceptualize gastroparesis and functional dyspepsia in a spectrum. Dr. Carbone and Dr. Grover will discuss emerging changes in diagnostic landscape including the use of surface mapping and pyloric assessments using FLIP and gastroduodenal manometry.
Part 3: Dr. Keszthelyi is a clinician-scientist and an authority in the area of treatment trials for GI motility disorders including gastroparesis and functional dyspepsia. Using case-based approach, Dr. Keszthelyi and Dr. Grover will discuss recent advancements in pharmacotherapy, gastric electrical stimulator and pyloric treatments. They will appraise data from both successful and failed clinical trials and how they can allow us to learn about the disease and plan future trials. Additionally, they will discuss how gastroparesis treatments of the future should be designed based on the emerging molecular data.
Presented by:
Madhusudan Grover, MD
Special Guests:
Prof. Daniel Keszthelyi, MD PhD
Florencia Carbone, PhD
Highlights of Lead Papers from the Rome Foundation Global Epidemiology Study
A Rome Foundation Continuing Medical Education program
The groundbreaking Rome Foundation Global Epidemiology Study (RFGES) has now published over 40 papers with many others in preparation.
It serves as the reference paper for practice and research on the Disorders of Gut-Brain Interactions (DGBI) and its initial paper “Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study” is now approaching 1,000 citations, making it the leading reference in the field.
In this session of the Rome Foundation Grand Rounds, we will present an introduction to the RFGES and its methodology and highlight three of its leading papers:
-Greater Overlap of Rome IV Disorders of Gut-Brain Interactions Leads to Increased Disease Severity and Poorer Quality of Life. Presenter, Ami Sperber
-Novel Irritable Bowel Syndrome Subgroups are Reproducible in the Global Adult Population. Presenter, Chris Black
-Symptom profiles compatible with disorders of gut-brain interaction (DGBI) in organic gastrointestinal diseases: A global population-based study. Presenter, Tom van Gils
Presented by:
Ami Sperber, MD, MSPH, RFF
Olafur Palsson, PsyD
Chris Black, PhD, MRCP
Tom van Gils, MD PhD

Grand Rounds 2024 - Scientific evidence for a central role of food in IBS
This symposium from the newly formed Rome Foundation Diet and Nutrition section provides updates about the scientific evidence that supports the relevance of food in symptom generation in IBS and the use of various dietary interventions in the management of patients with IBS.
The symposium starts with a general overview on the role of food in the pathophysiology with IBS by Rome Foundation Board Member Magnus Simrén, University of Gothenburg, Sweden, and continues with two lectures dedicated to the current dietary interventions used to treat symptoms in IBS by Caroline Tuck, Swinburne University, Australia and Stine Störsrud, University of Gothenburg, Sweden; the session ends with a general discussion and Q&A, and after the session attendees will have a better knowledge about the scientific basis for a central role for food in the pathophysiology in IBS, and for use of dietary approaches as part of the clinical management of IBS, and how to communicate this to the patients.
Presented by:
Magnus Simrén, MD, PhD, RFF
Carolina Tuck, PhD
Stine Störsrud, RD, PhD
Grand Rounds 2024 - Low FODMAP Diet Dilemmas: A Case-based Approach
This symposium will use a case-based approach to provide answers to questions that commonly arise about the low FODMAP diet when used for patients with IBS:
|
Presented by:
William D. Chey, MD, AGAF, FACG, FACP, RFF
Marvin Pollard, Professor of Gastroenterology, Professor of Nutrition Sciences
Chief, Division of Gastroenterology & Hepatology
Michigan Medicine, Ann Arbor, MI, USA
Nancee B. Jaffe, MS, RDN
Lead Dietitian for the UCLA Vatche and Tamar Manoukian Division of Digestive Diseases

Grand Rounds 2024: The 3 step approach to Integrated Psychosocial Care in DGBI
Objectives for this Grand Rounds include:
|
Presented by:
Laurie Keefer, PhD, RFF
Professor of Medicine and Psychiatry
Icahn School of Medicine at Mount Sinai
New York, NY, USA

Grand Rounds 2024: Abdominal Bloating and Distension
This Rome Foundation Grand Rounds presentation will appeal to individuals interested in evaluating and treating one of the most prevalent cluster of gastrointestinal symptoms – gas and bloating. These symptoms develop for a variety of different reasons. They are reported by a large number of patients with disorders of gut-brain interaction, such as irritable bowel syndrome and functional dyspepsia. The cause can be elusive; the pathophysiology is complex. The speaker will provide his perspective on this disorder, based on his clinical experience treating patients with these symptoms and research in the field.
Objectives for this Grand Rounds include:
● Review the epidemiology of abdominal bloating and distension
● Appreciate the complex pathophysiology of bloating and distension
● Recognize available treatment options
Speaker:
Brian E. Lacy, MD, PhD, FACG, RFF
Professor of Medicine & Senior Associate Consultant
Mayo Clinic, Jacksonville, FL, USA

Grand Rounds 2024: Ten Questions About Functional Dyspepsia (An Interactive Case-based Illustration of New Developments)
Functional dyspepsia is one of the most common and challenging conditions in clinical practice. The last few years have seen major evolutions in the understanding of the disease, its underlying pathophysiology, and the available treatment options. The separation from gastroparesis is an ongoing topic of transatlantic and international debate.
This interactive program will use a case-based approach to reveal some of the current concepts, ongoing controversies, and new information that is likely to be presented at meetings and in the literature later this year.
The program will appeal to clinicians, medical providers, and researchers interested in understanding the complexity of upper gastrointestinal symptoms, their relationship to physiological events such as food intake, and the potential impact of novel pharmacological and dietary therapeutic interventions.
Grand Rounds 2024: Abuse, Trauma, and Illness: What is the link?
A Rome Foundation Continuing Medical Education program
Presentation by Douglas A. Drossman, MD With special guests: Lin Chang MD & Johannah Ruddy MEd
This comprehensive program will appeal to individuals interested in unraveling the intricate interplay between abuse, trauma, and gastrointestinal illness.
Part 1 begins with a compelling case report by Dr. Drossman, recounting the journey of his adolescent patient who, having endured early trauma, developed gastrointestinal symptoms. This case spurred Dr. Drossman to pioneer the first study in the medical literature, elucidating this association.
Part 2, presented by Dr. Chang, offers an insightful research update, including her groundbreaking studies into the association between adverse childhood events and gastrointestinal illness, bringing us to the present day.
Part 3, presented by Ms. Ruddy, invites us into the realm of a patient’s experience.
Part 4 concludes the program as Dr. Drossman imparts his clinical experience and insights in caring for these patients to aid healthcare providers.

Grand Rounds: Communication Skills
Have you felt challenged when communicating with your patient or even frustrated that the visit just isn’t going well? Now you can learn Grand Rounds how to successfully navigate complex patient interactions, improving patient provider satisfaction and clinical outcome.
Douglas A. Drossman, MD, a recognized authority in DGBI and communication strategies, will present tips and techniques for optimizing the patient-provider relationship through the medical interview.
Objectives:
●Learners will understand how to provide patient centered care and improve upon shared decision making.
● Learners will understand the importance of effective communication skills to navigate challenging clinical situations
● Learners will understand the impact of DGBI from the patient’s perspective and learn their role in reducing the stigma experience for patients with DGBI

Grand Rounds: Sociocultural aspects of the assessment and treatment of patients with DGBI
A Rome Foundation Continuing Medical Education program Awareness and understanding of the sociocultural background of patients with DGBI can help avoid pitfalls and enhance the clinical outcome of patients with DGBI. The Multidimensional Clinical Profile (MDCP) approach, with unique case presentations, will be used to demonstrate how to navigate these complex issues in clinical practice.
Objectives:
● Recognize and assess the patient’s sociocultural background and its potential effect on the patient/HCP relationship and clinical outcome.
● Assess the effect of sociocultural factors on the patient’s “explanatorymodel of illness.”
● Recognize and bridge differences between the patient’s and the provider’s sociocultural backgrounds.
● Use the Multidimensional Clinical Profile (MDCP) approach to clinical practice including sociocultural influences.

Grand Rounds: Diet and DGBI
Introducing Rome Grand Rounds Session #4: Diet & DGBI
A virtual, interactive and intensive educational opportunity on topics related to Disorders of Gut-Brain Interaction (DGBI)
Each session will offer 1.25 CME credits and the opportunity to learn from the world’s best clinicians and researchers in the area of DGBI.
Objectives:
● Understand the role that food can play in symptom generation in patients with DGBI.
● Understand the impact that dietary therapies can play in symptom management
● Understand how the integrated care model, include dietary guidance, can improve clinical outcomes

Grand Rounds: Post Covid-19 DGBI
Introducing Rome Grand Rounds Session #7: Post Covid-19 DGBI
A virtual, interactive and intensive educational
opportunity on topics related to
Disorders of Gut-Brain Interaction (DGBI)
Each session will offer 1.25 CME credits and the
opportunity to learn from the world’s best clinicians and
researchers in the area of DGBI.
Objectives:
● To understand the mechanisms that explains the impact of SARS-CoV-2 in the GI tract.
● To understand the underlying pathophysiological mechanisms of the Post COVID-19 DGBI and learn the Diagnostic Criteria.”
● To learn the current studies that demonstrate the presence of Post COVID-19 DGBI.
● To review how the COVID-19 pandemic impacted in the practice of Neurogastroenterology especially in terms of Motility and DGBI.

Grand Rounds: Evidence supporting Brain-Gut Behavioral Therapies (BGBT) and Integrated Care to Improve access through Mental Health
Objectives:
● Be able to explain the evidence supporting integrated behavioral care in DGBI.
● Identify a model of integrated behavioral care that would a) work in your practice tomorrow and b) could be implemented in your practice over the next two years
● Be able to explain the strengths and limitations of digital technology as part of integrated behavioral DGBI care
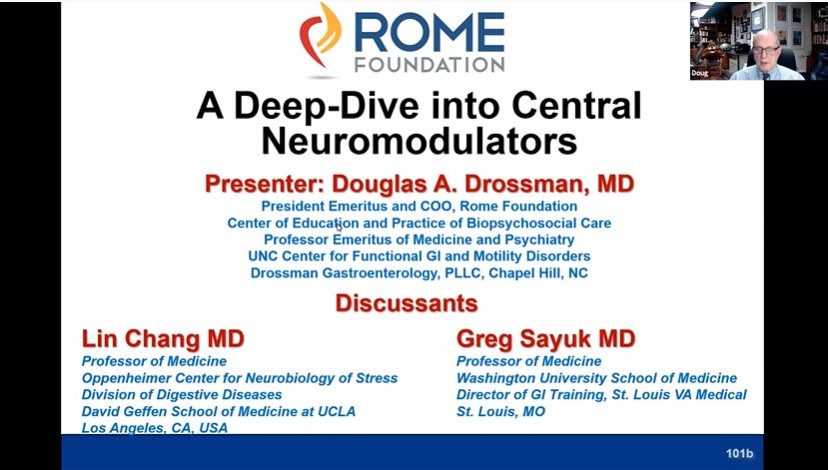
Grand Rounds: Deep Dive Into Central Neuromodulators
Objectives:
● Explained the pathophysiological basis for central neuromodulators in treating pain and other symptoms in patients with DGBI
● Determined treatment options for patients with DGBI symptoms, including abdominal pain

Grand Rounds: DGBI in Pediatric Populations
Objectives:
● Understand the pathophysiology of Pain Predominant Pediatric Disorders of Gut Brain Interaction (DGBI)
● Identify the utility for different treatments including non-pharmacologic and pharmacologic interventions
● Understand the multidisciplinary approach to the treatment of these patients

Grand Rounds: Gastroparesis vs FD
Objectives:
● To understand the pathophysiology of both Functional Dyspepsia with sub-categories and Gastroparesis
● To understand the overlapping mechanisms of both conditions, with and without nausea/vomiting
● To understand the recommendations for when/when not to use gastric emptying testing for diagnosis
● To understand the recommendations for treatment of both conditions
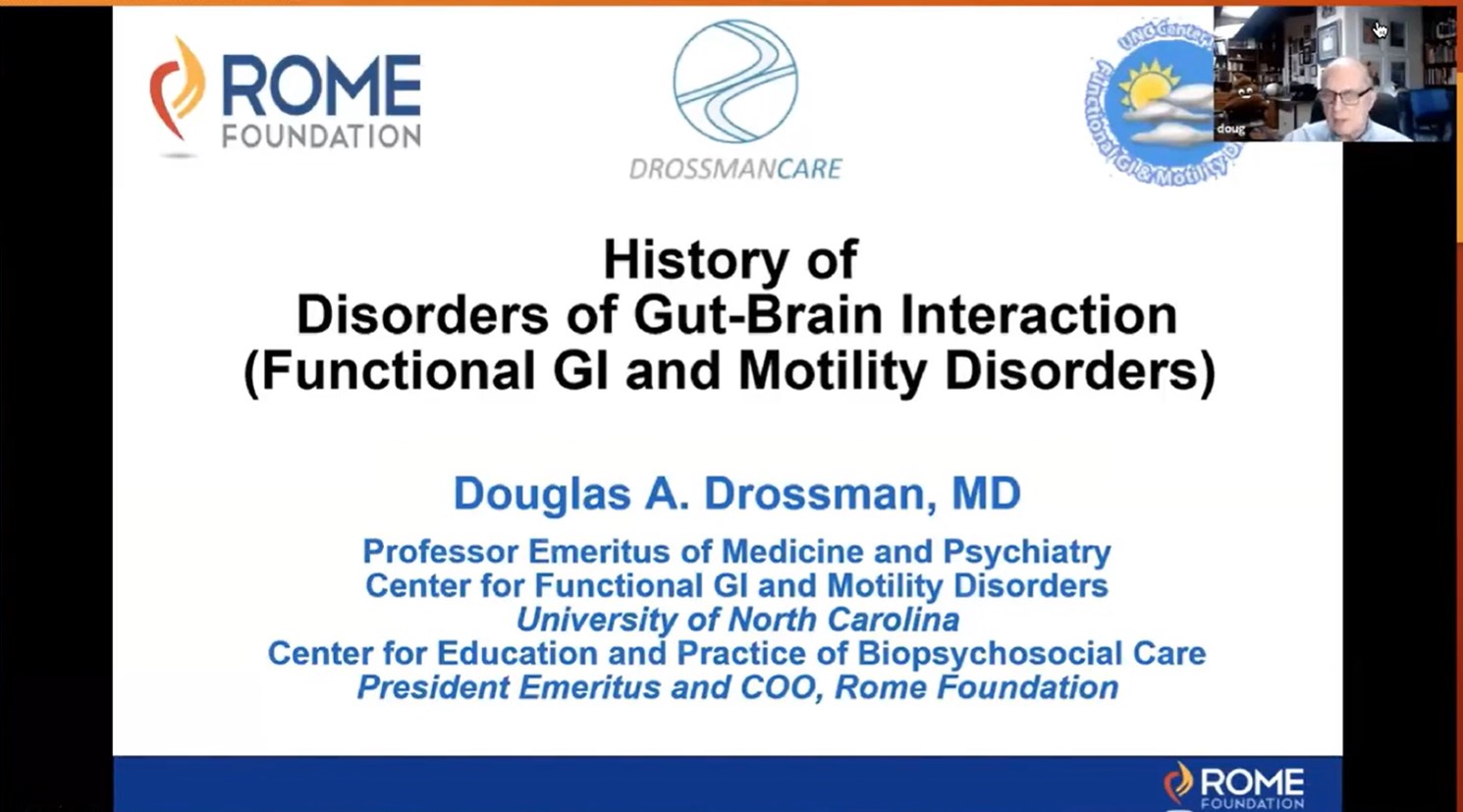
Grand Rounds: History of Disorders of Gut-Brain Interaction - DGBI (Functional GI Disorders)
This Grand Rounds features the original members of the Rome Foundation board who address the History of DGBI from the last millennia, to the present time. They also discuss the basis for the creation of the Rome Foundation.
Objectives:
● To understand the historical evolution of thinking about DGBI
● To understand the pathophysiological bases for DGBI
● Describe the historical evolution of thinking about DGBI
● Describe the pathophysiological bases for DGBI
● Trace the history of the formation of the Rome Foundation
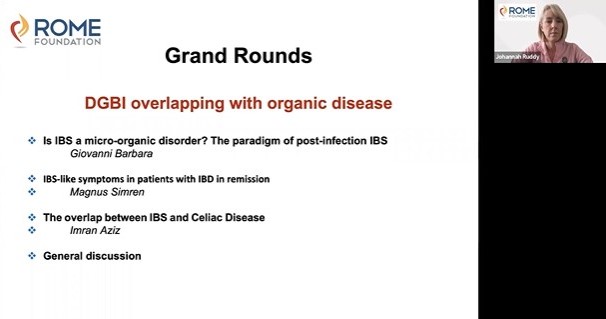
Grand Rounds: DGBI Overlapping with Organic Disease
Objectives:
● Describe the prevalence, GI symptom patterns and clinical impact of coexisting GI illnesses, assess potential geographic and demographic differences, and address how the presence of these symptoms relates to GI symptom patterns in specific DGBI.
● Provide guidance on how the presence of co-existing GI illnesses influences burden of the disease, clinical outcomes and patient management, including how to prioritize different treatment strategies.

Grand Rounds: Initial Approach to a Patient with Severe Chronic Abdominal Pain: How to Engage, Educate and Achieve Collaborative Care
This module shows the interaction with Ms. Byers a simulated patient with multiple diagnoses including:
● Post-infection IBS
● Opioid-induced constipation
● Narcotic Bowel Syndrome
● Centrally mediated abdominal pain
● Psychosocial difficulties including
- History of abuse and trauma
- Somatic symptom disorder
- Visceral anxiety
- Depression
- Opioid seeking behavior
This module is designed to help the provider understand these disorders, engage with the patient in an effective patient-provider relationship, and use good communication skills to recommend effective treatments.
Grand Rounds - Demystifying Gastroparesis: Lessons from Around the World copy 1
A Rome Foundation Continuing Medical Education program
Summary:
This discussion-style and interactive program will be geared towards practitioners and other individuals interested in learning about advancements in gastroparesis.
Objectives:
1. To understand the clinical spectrum of gastroparesis and differentiation from functional dyspepsia
2. To discuss the role of novel diagnostics such as gastric mapping, FLIP, and full-thickness biopsies
3. To appraise clinical trials and the future of drug development for gastroparesis
These presentations will be followed by a Q&A session and panel discussion.
Part 1: This will be a brief overview of gastroparesis epidemiology and clinical presentation by Dr. Grover. Working with the Gastroparesis Clinical Research Consortium, Dr. Grover has participated in over 60 clinical and translational studies in gastroparesis and is a leading authority on disease mechanisms. He has a busy practice of gastroparesis patients. He will share recent epidemiological studies as well as insights on clinical presentation.
Part 2: Dr. Carbone is an internationally recognized researcher in GI motility disorders and played key roles in developing international consensus statements on gastroparesis and functional dyspepsia. Using a case-based approach, Dr. Carbone will lead discussion on the diagnosis of gastroparesis, challenges with gastric emptying study and how to conceptualize gastroparesis and functional dyspepsia in a spectrum. Dr. Carbone and Dr. Grover will discuss emerging changes in diagnostic landscape including the use of surface mapping and pyloric assessments using FLIP and gastroduodenal manometry.
Part 3: Dr. Keszthelyi is a clinician-scientist and an authority in the area of treatment trials for GI motility disorders including gastroparesis and functional dyspepsia. Using case-based approach, Dr. Keszthelyi and Dr. Grover will discuss recent advancements in pharmacotherapy, gastric electrical stimulator and pyloric treatments. They will appraise data from both successful and failed clinical trials and how they can allow us to learn about the disease and plan future trials. Additionally, they will discuss how gastroparesis treatments of the future should be designed based on the emerging molecular data.
Presented by:
Madhusudan Grover, MD
Special Guests:
Prof. Daniel Keszthelyi, MD PhD
Florencia Carbone, PhD
Highlights of Lead Papers from the Rome Foundation Global Epidemiology Study copy 1
A Rome Foundation Continuing Medical Education program
The groundbreaking Rome Foundation Global Epidemiology Study (RFGES) has now published over 40 papers with many others in preparation.
It serves as the reference paper for practice and research on the Disorders of Gut-Brain Interactions (DGBI) and its initial paper “Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study” is now approaching 1,000 citations, making it the leading reference in the field.
In this session of the Rome Foundation Grand Rounds, we will present an introduction to the RFGES and its methodology and highlight three of its leading papers:
-Greater Overlap of Rome IV Disorders of Gut-Brain Interactions Leads to Increased Disease Severity and Poorer Quality of Life. Presenter, Ami Sperber
-Novel Irritable Bowel Syndrome Subgroups are Reproducible in the Global Adult Population. Presenter, Chris Black
-Symptom profiles compatible with disorders of gut-brain interaction (DGBI) in organic gastrointestinal diseases: A global population-based study. Presenter, Tom van Gils
Presented by:
Ami Sperber, MD, MSPH, RFF
Olafur Palsson, PsyD
Chris Black, PhD, MRCP
Tom van Gils, MD PhD

Grand Rounds 2024 - Scientific evidence for a central role of food in IBS copy 1
This symposium from the newly formed Rome Foundation Diet and Nutrition section provides updates about the scientific evidence that supports the relevance of food in symptom generation in IBS and the use of various dietary interventions in the management of patients with IBS.
The symposium starts with a general overview on the role of food in the pathophysiology with IBS by Rome Foundation Board Member Magnus Simrén, University of Gothenburg, Sweden, and continues with two lectures dedicated to the current dietary interventions used to treat symptoms in IBS by Caroline Tuck, Swinburne University, Australia and Stine Störsrud, University of Gothenburg, Sweden; the session ends with a general discussion and Q&A, and after the session attendees will have a better knowledge about the scientific basis for a central role for food in the pathophysiology in IBS, and for use of dietary approaches as part of the clinical management of IBS, and how to communicate this to the patients.
Presented by:
Magnus Simrén, MD, PhD, RFF
Carolina Tuck, PhD
Stine Störsrud, RD, PhD

GastroPsych Clinical Case Conference Series
A Rome Foundation Continuing Medical Education program
Patients with a wide range of gastrointestinal conditions, including functional bowel disorders, gastroparesis, chronic pancreatitis, esophageal conditions, and inflammatory bowel disease may experience brain-gut dysregulation that can impact their symptoms and/or disease experience. In an engaging and practical case series, leading experts in psychogastroenterology will discuss how to utilize psychological interventions with complex and unique GI presentations. Click on the specific session link below to register for that session.
Session One: Psychological Care for Adults with Chronic Pancreatitis
Session Two: Behavioral Treatment for Sleep Disturbance in DGBIs
Session Three: Psychological Intervention with Adolescent/Young Adult Patients with DGBIs
Session Four: Behavioral Medicine Interventions for Eosinophilic Esophagitis
Session Five: Psychological Treatment Strategies for Cyclic Vomiting Syndrome
Session Six: Case Conceptualization and Cognitive-Behavioral Treatment for Avoidant Restrictive Food Intake Disorder
Session Seven: Acceptance and Commitment Therapy with a patient with Inflammatory Bowel Disease and an Ostomy
Session Eight: GI illness and Sexual Dysfunction
CE Credits: 1 hour of continuing education credit for Licensed Psychologists will be awarded for each seminar. There is no cost to attend. Attendees must complete each seminar's associated evaluation form in order to receive credit.
GastroPsych - Integrating Group Therapy into GI Behavioral Health Practice
A Rome Foundation Continuing Medical Education program
- Describe the empirical data supporting group treatment for GI symptoms
- List two logistical components of integrating groups into practice.
- Identify two benefits of offering group treatment for GI patients.
- Explain two clinical challenges that might arise in providing group treatment for GI patients, and how to address each.
Grand Rounds 2024 - Low FODMAP Diet Dilemmas: A Case-based Approach
This symposium will use a case-based approach to provide answers to questions that commonly arise about the low FODMAP diet when used for patients with IBS:
|
Presented by:
William D. Chey, MD, AGAF, FACG, FACP, RFF
Marvin Pollard, Professor of Gastroenterology, Professor of Nutrition Sciences
Chief, Division of Gastroenterology & Hepatology
Michigan Medicine, Ann Arbor, MI, USA
Nancee B. Jaffe, MS, RDN
Lead Dietitian for the UCLA Vatche and Tamar Manoukian Division of Digestive Diseases

Grand Rounds: The 3 step approach to Integrated Psychosocial Care in DGB
Objectives for this Grand Rounds include:
|
Presented by:
Laurie Keefer, PhD, RFF
Professor of Medicine and Psychiatry
Icahn School of Medicine at Mount Sinai
New York, NY, USA

Grand Rounds: Abdominal Bloating and Distension
This Rome Foundation Grand Rounds presentation will appeal to individuals interested in evaluating and treating one of the most prevalent cluster of gastrointestinal symptoms – gas and bloating. These symptoms develop for a variety of different reasons. They are reported by a large number of patients with disorders of gut-brain interaction, such as irritable bowel syndrome and functional dyspepsia. The cause can be elusive; the pathophysiology is complex. The speaker will provide his perspective on this disorder, based on his clinical experience treating patients with these symptoms and research in the field.
Objectives for this Grand Rounds include:
● Review the epidemiology of abdominal bloating and distension
● Appreciate the complex pathophysiology of bloating and distension
● Recognize available treatment options
Speaker:
Brian E. Lacy, MD, PhD, FACG, RFF
Professor of Medicine & Senior Associate Consultant
Mayo Clinic, Jacksonville, FL, USA

Grand Rounds: Ten Questions About Functional Dyspepsia (An Interactive Case-based Illustration of New Developments)
Functional dyspepsia is one of the most common and challenging conditions in clinical practice. The last few years have seen major evolutions in the understanding of the disease, its underlying pathophysiology, and the available treatment options. The separation from gastroparesis is an ongoing topic of transatlantic and international debate.
This interactive program will use a case-based approach to reveal some of the current concepts, ongoing controversies, and new information that is likely to be presented at meetings and in the literature later this year.
The program will appeal to clinicians, medical providers, and researchers interested in understanding the complexity of upper gastrointestinal symptoms, their relationship to physiological events such as food intake, and the potential impact of novel pharmacological and dietary therapeutic interventions.
Grand Rounds: Abuse, Trauma, and Illness: What is the link?
A Rome Foundation Continuing Medical Education program
Presentation by Douglas A. Drossman, MD With special guests: Lin Chang MD & Johannah Ruddy MEd
This comprehensive program will appeal to individuals interested in unraveling the intricate interplay between abuse, trauma, and gastrointestinal illness.
Part 1 begins with a compelling case report by Dr. Drossman, recounting the journey of his adolescent patient who, having endured early trauma, developed gastrointestinal symptoms. This case spurred Dr. Drossman to pioneer the first study in the medical literature, elucidating this association.
Part 2, presented by Dr. Chang, offers an insightful research update, including her groundbreaking studies into the association between adverse childhood events and gastrointestinal illness, bringing us to the present day.
Part 3, presented by Ms. Ruddy, invites us into the realm of a patient’s experience.
Part 4 concludes the program as Dr. Drossman imparts his clinical experience and insights in caring for these patients to aid healthcare providers.
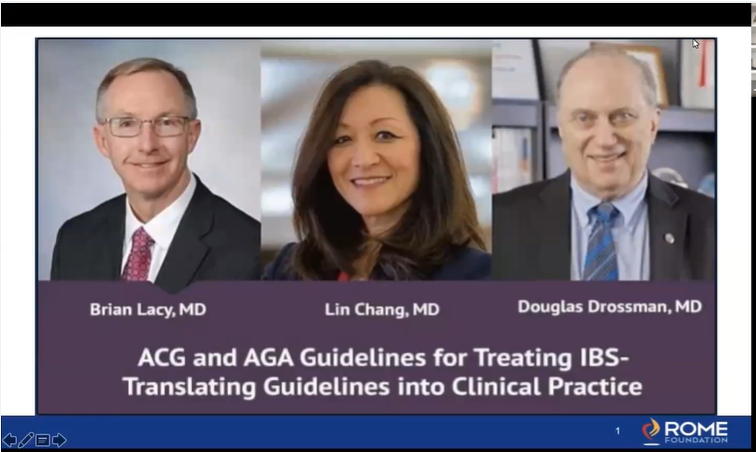
Grand Rounds: ACG vs AGA IBS Guidelines and Clinical Application
Objectives:
● Learners will understand the rationale for the IBS guidelines from the AGA and ACG
● Learners will understand how to adapt the guidelines to real world application to make appropriate diagnosis and treatment
Rome Foundation Virtual Pediatric Symposium - 0 CE Credits
Learn how to manage pediatric Disorders of Gut-Brain Interaction: newborns through adolescents. This symposium will teach the process of evaluation, diagnosis and treatment. In addition we will bring in the complex nature of including the role of the family in management of pediatric patients with DGBI.
The Rome Foundation Forums
The Rome Foundation forums are spaces where professionals can meet and discuss the clinical and scientific topics related to Disorders of Gut-Brain Interaction (DGBI).
- Discuss the clinical and scientific intersection of psychology and gastroenterology in the GastroPsych forum.
- In the Grand Rounds forum, professionals can meet and discuss the clinical and scientific topics related to Disorders of Gut-Brain Interaction (DGBI).
We value open, thoughtful, and respectful discussions. To maintain a supportive and productive environment, we ask all members to:
● Be Respectful: Treat others with kindness and professionalism. Disagreements are natural, but please focus on the ideas and not the individual. Avoid personal attacks, inflammatory remarks, or unprofessional behavior.
● Maintain Professionalism: This forum is about topics related to Disorders of Gut-Brain Interaction (DGBI). Keep discussions relevant, accurate, and based on scientific evidence when applicable.
● Be Supportive: We’re here to learn from each other. Offer constructive feedback and encouragement to foster a positive community.
● Respect Privacy: Do not share personal or patient information in any form. Uphold confidentiality and adhere to HIPAA and other relevant privacy laws.
By participating in this forum, you agree to abide by these guidelines. Let’s work together to create a respectful and enriching environment for everyone.
Thank you for your cooperation!